Annex - About NHS Continuing Healthcare
NHS CHC is care provided to someone who has complex care needs. The care can be provided in someone’s own home, a care home or other place outside of a hospital. This care is paid for by the NHS and covers the full cost of the person’s care and residential needs.
Eligibility for NHS CHC funding is determined by whether a person has a ‘primary health need’. This means that the main aspects of the care they require are focused on addressing health needs. Having a primary health need is not about the reason why an individual requires care or support, nor is it based on their diagnosis; it is about the level and type of their overall actual day-to-day care needs taken in their totality.
Local CCGs are at the frontline of NHS CHC, as they are responsible for assessing people’s needs, and arranging and funding care. CCGs do this under the National Framework. The National Framework is underpinned by the Standing Rules regulations, which require CCGs to follow it.
The National Framework was first published in 2007 and sets out the process CCGs should follow to determine eligibility for NHS CHC and arrange appropriate care. It provides a checklist for initial screening as well as a detailed decision support tool for NHS CHC practitioners to use when assessing whether someone is eligible for NHS CHC funding.
The scale of NHS CHC in England
In 2015-16, NHS CHC cost CCGs £3.6billion, and by 2020-21 was expected to cost £5.2billion. However, savings have been made in the administration of NHS CHC and growth has not been as fast as previously anticipated. In 2018-19, NHS CHC cost approximately £3.7billion. Although savings have been made and growth in spending is slower than had been expected, it still represents approximately 4% of CCG spending. There is no cap on NHS CHC funding, which means all those eligible should receive the funding they need.
According to NHS England and NHS Improvement, these savings have been made without any changes to eligibility. In 2015-16, almost 160,000 people were eligible for NHS CHC funding and in 2019-20, this figure was 166,000. The proportion of those referred to CCGs for consideration who are eligible for NHS CHC funding has remained fairly constant: in 2015-16, 18% of those referred were eligible and in 2019-20, 19% were eligible.
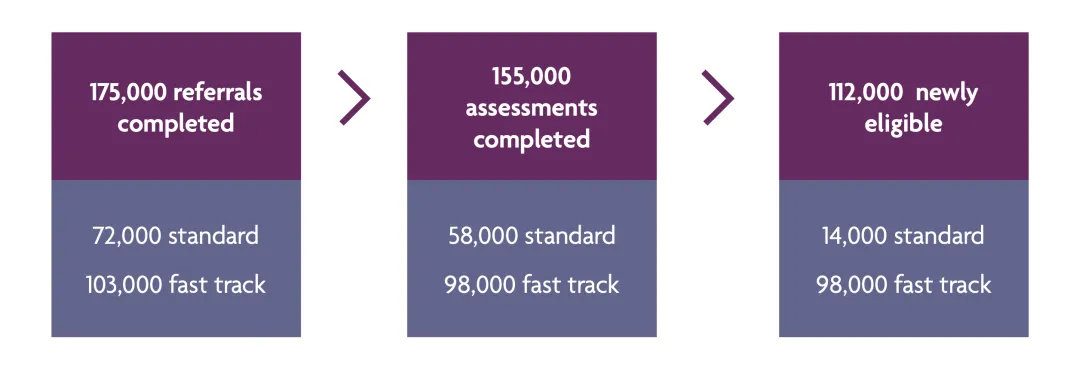
NHS CHC is split between ‘standard’ CHC for people with a primary health need and ‘fast track’ for people with a rapidly deteriorating illness that may be entering a terminal phase. The majority (87.5%) of people who are eligible for NHS CHC funding are on the fast track. There are different processes in place for each type. People referred for standard NHS CHC go through a more detailed assessment process. The fast track process is more streamlined allowing a suitable clinician to determine a person’s eligibility.
Figure 3: NHS CHC eligibility 2019-20
In 2019-20, there were 3,327 reviews of eligibility completed by CCGs, 4.6% of the total referrals (though these are not directly related as the reviews may be for decisions made in previous years). Of these, 588 (18%) resulted in eligibility.
Who does what
The Department of Health and Social Care produces the National Framework for Continuing Healthcare and NHS Funded Nursing Care. It last updated the National Framework in 2018.
CCGs are at the frontline of NHS CHC in England. CCGs are responsible for screening referrals and assessing eligibility for NHS CHC funding.
For standard NHS CHC funding, this is a two-stage process:
- on referral, CCGs will screen using the NHS continuing healthcare checklist
- CCGs will then carry out a full assessment to decide on eligibility, using the NHS continuing healthcare decision support tool. This requires the input of a Multidisciplinary Team (MDT).
Once a person’s eligibility for NHS CHC funding is confirmed, the CCG is then responsible for care planning, service commissioning and case management. This includes regular reviews of care needs.
CCGs are also responsible for undertaking reviews of eligibility and must have a local resolution process set out. This includes requests to review previously unassessed periods of care. If a case cannot be resolved locally, the individual can seek an independent review.
NHS England and NHS Improvement is responsible for undertaking the independent review of eligibility decisions. This process includes taking the case to an Independent Review Panel.
If the person is dissatisfied with the decision of the Independent Review Panel, they can follow the NHS Complaints Procedure and bring a complaint to the Parliamentary and Health Service Ombudsman.
The review process is free for people who need to use it. Nonetheless, people sometimes need support. Every area in England has an independent NHS complaints advocacy service funded by the local authority. They can help people make a complaint about the NHS. There are a number of providers, and local Healthwatch organisations can provide details.
Additionally, NHS England and NHS Improvement has funded Beacon to provide a free advice service, allowing up to 90 minutes of information and support to help people trying to navigate the NHS CHC system.
Some firms, such as Beacon, operate services supporting people to pursue claims for NHS CHC funding. This can be on an hourly rate or a no-win-no-fee basis. There is no requirement for people to use a paid-for service to seek an NHS CHC review.
PHSO’s previous work and the evolution of NHS CHC since 1994
In 1994, the then Ombudsman published a report of an investigation about a health authority’s failure to provide long term care for a man who had brain damage. We found that the health authority had a policy not to provide care for people with a neurological condition.
Following this, in 1996 the then Ombudsman published a report containing five similar cases. These cases highlighted the impact of poor local arrangements for people requiring long term care because of a primary health need, where national guidance had not been followed.
In between these two reports, the Department of Health put in place the first national guidance for local health authorities. This guidance did not provide a national set of eligibility criteria, but did require local written policies and criteria, and listed the type of needs that should be covered.
In 1999, a legal case known as the Coughlan Judgement put in law the principle that if a person’s need was primarily health based, responsibility for that person’s care lied with the NHS. To reflect this, the Department of Health updated the national guidance both immediately after the Coughlan Judgement and again in 2001, to take account of its findings.
In 2003, we published the first of three linked reports on NHS CHC, as a result of an increase in the numbers of complaints we were receiving. This report looked at cases dating between 1997 and 2001. We found that national guidance had not provided the secure foundation needed for a fair and transparent system. The guidance that did exist had been misinterpreted and misapplied.
In the 2003 report, we recommended the Department of Health and health authorities review the criteria used between 1996 and 2002 and make efforts to right any financial wrongs. We also recommended that the Department of Health review the national guidance to make it clearer where the NHS must fund care.
Following the 2003 report, the Ombudsman received 4,000 complaints and the Department of Health set aside £180 million to fund retrospective claims.
In 2004, the then Ombudsman published a follow up report, which looked at how local NHS organisations had processed the retrospective reviews brought about by her 2003 report. This reiterated the need for clear national guidance and support for local NHS organisations to apply eligibility criteria. In response, the Department of Health announced it would be developing a nationally consistent approach.
In 2006 another legal case, known as the Grogan Judgement, highlighted further criticisms of the national guidance and local variance in eligibility criteria.
In 2007, the Department of Health published the first version of the National Framework, introducing national eligibility criteria, processes, and tools to support decision making. This was followed in 2009 by a revised framework establishing a fast track for people with a rapidly deteriorating condition.
Also in 2007, we published a further report, looking at how the Department of Health had established redress for those found eligible as a result of our 2003 report. We found the Department had made a mistake in how it decided to calculate the amount people were entitled to, taking no account of the actual costs to people and the impact of the previous system.
The Department of Health published a revised National Framework in 2012 to take account of structural changes in the NHS, notably the introduction of Clinical Commissioning Groups in place of the previous Primary Care Trusts. As part of this, in 2012 the Department put in place a series of deadlines for people to request a review of a previously unassessed period of care covering the period 1 April 2004 to 31 March 2012. This was intended to give CCGs a clear slate for NHS CHC assessments and ensure there was a limited backlog of claims.
NHS England and NHS Improvement is currently undertaking the Continuing Healthcare Strategic Improvement Programme. This will run until 2021 and aims to:
- reduce the variation in patient and carer experience of NHS CHC assessments, eligibility and appeals
- ensure that assessments occur at the right time and place, with fewer assessments taking place in hospitals
- work with CCGs across the country to identify best practice that can be adopted by other CCGs
- set national standards of practice and outcome expectations.
- make the best use of resources – offering better value for patients, the population and the taxpayer
- strengthen the alignment between other NHS England and NHS Improvement work programmes which have a CHC component, such as Personalisation and Choice.
The Continuing Healthcare Strategic Improvement Programme has led to the development of the NHS CHC e-learning tool and the CHC Competency Framework for frontline staff in CCGs. Apprenticeships schemes and a level 7 Open University qualification are also in development. The Continuing Healthcare Strategic Improvement Programme seeks to address the issues raised in recent years by organisations such as the National Audit Office and the Continuing Healthcare Alliance (see below).
In 2018, the Department of Health and Social Care published a revised National Framework. This did not change any of the eligibility criteria but was designed to provide greater clarity around the assessment process, the role of CCGs and local authorities, and reflect some legislative changes. Specifically, the changes included:
- setting out that the majority of NHS CHC assessments should take place outside of acute hospital settings
- providing additional advice for staff on when individuals do and do not need to be screened for NHS CHC in order to reduce unnecessary assessment processes and provide greater clarity on this
- clarifying that the main purpose of three and 12-month reviews is to review the appropriateness of the care package, rather than reassess eligibility. This should reduce unnecessary re-assessments
- introducing new principles for CCGs regarding the local resolution process for situations where individuals request a review of an eligibility decision. The aim is to resolve such situations earlier and more consistently
- providing clearer guidance, including dedicated sections, on: the roles of CCGs and local authorities, NHS-funded Nursing Care, inter-agency disputes, well-managed needs, and the Fast Track Pathway Tool.
During the COVID-19 crisis of spring and summer 2020, all new NHS CHC assessments were paused to allow CCGs the flexibility and extra capacity to manage the additional pressures on the NHS. This meant the NHS funded all care for people who would otherwise have been referred for an NHS CHC assessment, and assessments were deferred. Assessments were restarted on 1 September, both for new referrals and for those deferred. Additional guidance was introduced to support CCGs to carry out these assessments.
NHS England and NHS Improvement has also developed a programme of work to support CCGs with the deferred assessments, including supporting the workforce, and securing additional resources for CCGs to increase capacity as well as providing additional e-learning material.
- 1994 – PHSO report Failure to Provide Long Term NHS Care for a Brain-Damaged Patient
- 1996 – PHSO report Investigations of Complaints about Long Term Health Care
- 1999 – The Coughlan judgement
- 2003 – PHSO report NHS Funding for Long Term Care
- 2004 - PHSO follow-up report NHS Funding for Long Term Care
- 2006 – The Grogan judgement
- 2007 – PHSO report Retrospective Continuing Care Funding and Redress
- 2007 – National Framework for NHS Continuing Healthcare and NHS-Funded Nursing Care
- 2009 – Revised National Framework for NHS Continuing Healthcare and NHS-Funded Nursing Care published, establishing the fast track for people with a rapidly deteriorating condition
- 2012 – Revised National Framework for NHS Continuing Healthcare and NHS-Funded Nursing Care published
- 2012-2013 Deadlines imposed for reviews of previously unassessed periods of care between 2004 and 2012
- 2016 – CHC Alliance report, Continuing to Care? Is NHS Continuing Healthcare Supporting the People Who Need it in England?
- 2016 – NAO Investigation into NHS Continuing Healthcare Funding
- 2017-2018 – Equalities and Human Rights Commission considered legal action against CCGs which had blanket caps on funding
- 2018 – Public Accounts Committee report on Continuing Healthcare
- 2018 – Revised National Framework for NHS Continuing Healthcare and NHS-Funded Nursing Care published
- 2020 – COVID-19 response paused new NHS CHC assessments between March and September
What others have said
Several other organisations have looked at issues with NHS CHC in recent years.
National Audit Office and Public Accounts Committee
The National Audit Office (NAO) is the UK’s independent public spending watchdog and supports Parliament in holding the Government to account. It helps improve public services through high-quality audits. NAO reports into Parliament’s Public Accounts Committee (PAC), which scrutinises public spending and holds the Government to account.
In 2017, NAO published its investigation into NHS continuing healthcare funding. NAO found that the assessment process raises people’s expectations that they will receive funding. They noted that only 18% of initial screenings result in a person being assessed as eligible.
NAO noted that NHS CHC was a significant cost pressure on CCGs’ spending, but that there is local variation in the number and proportion of people assessed as eligible. It said this variation could not be explained by population differences, meaning that it was likely there were differences in how CCGs interpreted and applied the National Framework and eligibility criteria.
NAO also noted there were limited assurance processes to ensure consistency in decision making at CCGs, and that there was a shortage of data on NHS CHC.
Following the NAO report, PAC held an inquiry and published its report in 2018. PAC largely echoed NAO’s findings. It found that people waited too long to find out if they were eligible and that some people did not receive the care they were entitled to because of a complex system. PAC also found too much local variation in the interpretation of the National Framework and its assessment tools.
Continuing Healthcare Alliance
The Continuing Healthcare Alliance is a group of 17 charities and organisations that share a belief that NHS CHC needs to improve. Continuing Healthcare Alliance members include Parkinson’s UK, Age UK, Marie Curie, Beacon, Carers Trust, Patients Association and other charities and organisations that have an interest in NHS CHC.
In 2016, the Continuing Healthcare Alliance published Continuing to care? Is NHS continuing healthcare supporting the people who need it in England?. In this report, the Alliance made a series of recommendations for national and local organisations to ensure improvement in NHS CHC:
- ensure multidisciplinary teams are composed of professionals who are experienced when making decisions around NHS CHC, with knowledge of the person, their condition(s), needs and aspirations
- design and deliver a mandatory programme of training for professionals who organise and assess people for NHS CHC to ensure they understand the eligibility criteria and how to use the current decision tools
- rewrite the checklist and Decision Support Tool so they more effectively measure individuals’ healthcare needs against the lawful limit of care that the local authority can provide
- introduce an option for professionals to select if they agree someone should not be reassessed for eligibility of NHS CHC. For people marked down as permanently eligible, reviews should only look at changing needs, for example, where someone may need increased support
- prevent people with long-term, serious health conditions being forced into residential care, or living at home with unsafe levels of care, by ensuring packages of care are needs-driven and not purely financially motivated
- publish data on how many people apply for NHS CHC – whether they are successful or not – as well as the number of people who proceed past the checklist stage to the full assessment.
Equalities and Human Rights Commission
The Equalities and Human Rights Commission (EHRC) is Great Britain’s national equality body. It works to safeguard and enforce the laws that protect people’s rights to fairness, dignity and respect.
In 2017, EHRC looked at taking legal enforcement action against CCGs having become concerned about CCGs having blanket policies with arbitrary caps on funding. EHRC said that such policies failed to consider individual needs, such as living location and family life, and were a breach of the Human Rights Act and the Public Sector Equality Duty.
EHRC wrote to 43 CCGs asking for more details about their approach, before initiating judicial review proceedings against 13 CCGs. These 13 CCGs subsequently reviewed their policies.